Summary
Why Lower Limb Alignment Matters in Knee OA
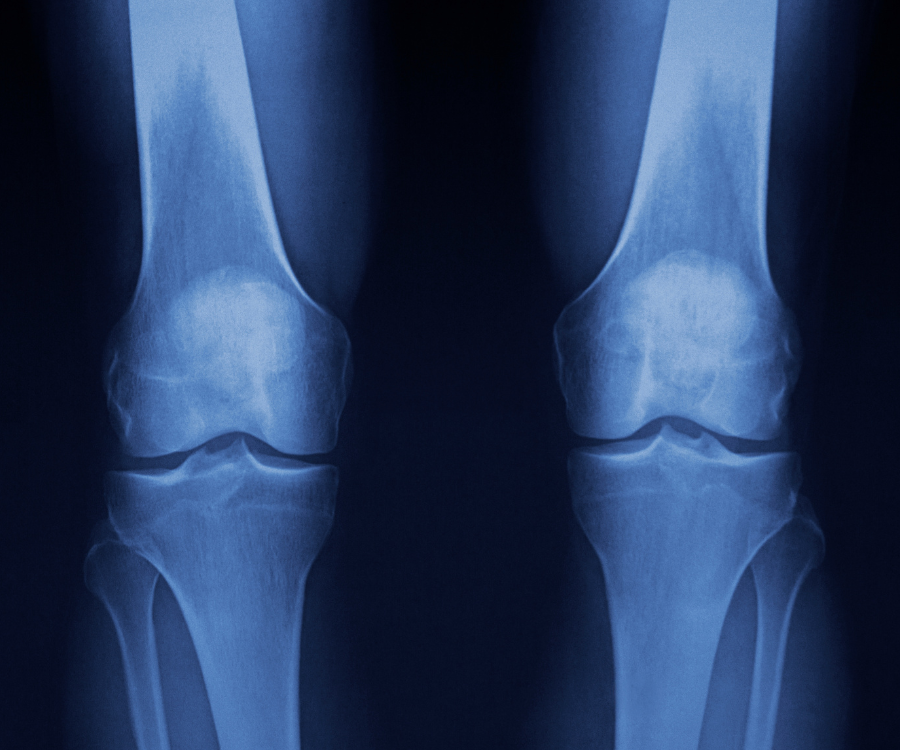
Frontal plane lower limb alignment is a key factor in assessing severity and informing clinical decision-making related to knee osteoarthritis treatments. Varus malalignment (inward angulation) or valgus malalignment (outward angulation) can accelerate disease progression and influence surgical decisions.
Current standard: Long-leg radiographs are used to measure alignment, but these have limitations:
- Radiation exposure from hips to ankles
- Inconsistent limb positioning and sex can alter results
- Static only — missing how alignment changes under load during gait
Dynamic assessment, such as measuring alignment while walking, can give a more complete picture of functional knee status.
The Promise of Markerless Motion Capture
Traditional motion capture systems require reflective markers and tight clothing, making them impractical for many clinics. Markerless systems like Theia3D use synchronized video cameras and deep learning to estimate whole-body 3D pose directly from individuals in regular clothing, without physical markers.
Advantages include:
- No radiation exposure
- Faster setup and assessment
- Applicable in both static and dynamic tasks
Previous validation work has shown Theia3D to have high repeatability and close agreement with marker-based systems.
Study Overview
Objectives:
- Quantify static and dynamic lower limb alignment in patients with advanced medial or lateral knee OA.
- Examine sex differences in alignment.
- Explore correlation between static (quiet standing) and dynamic (gait) alignment.
Participants:
- 92 patients (37 male, 55 female) with advanced knee OA (Kellgren-Lawrence grade 3+)
- 83 medial knee OA
- 9 lateral knee OA
Methods:
- Static task: Quiet standing for 30 seconds with standardized foot placement
- Dynamic task: Walking back and forth over 12 m for ~1 minute at self-selected speed
- Technology: Eight synchronized video cameras processed in Theia3D
- Measure: Frontal plane knee adduction angle (KAA), where >0° = varus, <0° = valgus
Key Findings
- Clear Separation Between Medial and Lateral OA
- Quiet standing: Medial OA averaged +3.1° varus, lateral OA averaged -4.3° valgus (p<0.001)
- Gait (first half of stance): Medial OA averaged +5.8° varus, lateral OA averaged -2.5° valgus (p<0.0001)
- Sex Differences
- Males were more varus than females in both static and dynamic tasks (p<0.01).
- Strong Static-Dynamic Correlation
- Spearman’s ρ = 0.86 (p<0.0001)
- On average, patients were 2.6° more varus during gait compared to quiet standing, regardless of their varus/valgus alignment during quiet standing.
- Clinical Insight
- Dynamic gait assessment revealed greater malalignment than static measures, highlighting the potential for varus thrust (worsening of varus alignment during single limb support).
Why This Matters for Clinicians
- Dynamic alignment assessment may capture functional deficits that static X-rays miss.
- Markerless systems can be integrated into clinic workflows with minimal setup.
- Potential for radiation-free, repeatable, and real-world assessments to guide treatment planning.
Limitations & Next Steps
- No direct X-ray comparison in this study, as this was not standard clinical practice.
- Smaller sample size for lateral OA reflects real-world prevalence but limits group balance.
Future research could integrate radiographic, markerless, and patient-reported outcomes to refine diagnostic pathways.
Read the full peer-reviewed study here.
Curious what these findings could mean for your clinic or lab?
Book a free Quick Consult with our biomechanics team to explore how markerless motion capture can fit into your workflows →